Occupation refers to functional tasks or activities that bring meaning to your life. And our children’s main activity is PLAY. Did you know that kids play to learn and that play requires motor, sensory processing, cognitive, and social skills? All these skills work together for learning. However, when the necessary skills for play are observably difficult, it can make grasping new competencies challenging for kids.
Occupational therapy addresses all the skills needed for play. It works on strength, coordination, and control to support their movement. OT also helps with sensory processing difficulties by identifying the way your toddler receives or responds to sensory input and teaching fun ways for you to support your child. And finally, Occupational Therapy promotes executive function skills building on motor, attention, and regulation foundations for learning.
Though play can look different and vary from child to child, there are general toddler development skill ranges necessary for learning to happen. When these are not progressing or missing, they can inhibit engaging in and learning through play.
The development of sensory processing and motor skills begins immediately at birth. The brain is where all the magic happens. Newborns take in sensations, but their body is unable to organize them—their reflexes are neurological responses to stimulation, including the senses of light, sound, touch, or pressure input such as stroking and vestibular sensory input with sudden movement.
The sensory processing and motor skill development looks random and clumsy at first with the baby’s initial kicking of their legs or trying to find their mouth with their hand. As they continue to be exposed to the sensation and repeat the movement, it becomes more purposeful.
Babies are holding, pulling, pushing, and dropping toys as they learn about cause and effect. More and more skills work together to explore and learn through play.
For your toddler, the years from 1 to 3 are very busy. They are essential years of curiosity, trial and error, and learning about what they can do. At age one, toddlers are very active. Give them a container, and everything comes out; maybe a few things go back inside. Set something on the table, and they pull up to see if they can get it. They make sounds and babble and may tug on your heart with Ma Ma or Da Da words!
Toddlers are in a transition of building more independence. During the terrible twos, a stage that everyone stresses about, they continue to learn about their environment, manipulate things, and communicate their experiences. Their development takes all the work that the baby’s brain and body did and uses it in play to build confidence, control movement, and explore new sensations. Toddlers experience big emotions. They must learn about these feelings and how their body responds to them. How we react and support them is important.
They also learn to transition from one activity to another, even when they don’t want to.
For example, two-year-olds usually can stack a few blocks, string a few large beads on a shoelace, feed themselves with a spoon, drink from an open cup or a straw, remove/pull on clothing, brush teeth, help wash their body at bath time, jump, run, and walk up and down a few steps. They can also throw a small ball toward a target, help clean up, and put toys away. Though the terrible twos try on parents and toddlers, they don’t last long. And both parents and kids learn a great deal!
As we strive to develop more patience during these times, our toddlers are growing far more in their quest for independence. Two-year-olds should be able to attend and learn a new play activity for 4-6 minutes. Some research even suggests that this age group should be able to focus on a task for 10 minutes.
Though many toddlers can sit and play for extended periods of time with preferred toys or activities they have initiated themselves, a better learning opportunity is to give them a new task to work on to develop manipulation skills like using a tool to scoop, fill a container, feed themselves with a spoon or fork, stack or build with blocks, lace beads on a string, or roll a ball back and forth.
Notice how your child works through activities. When development is not smooth, there will be clues in how your child moves, plays, speaks, or acts. See if you observe any of these challenges:
- unable to manipulate toys in play, they continue to dump, empty containers, or throw them around the room
- difficulty using tools to scoop, squeeze, hammer, draw
- unable to demonstrate repetitive play activities. May run around, only roll the car back and forth
- moves between many play activities quickly, not engaging in any of them
- requiring or demanding your attention and unable to initiate or engage in play by themselves for short periods
- difficulty imitating actions in movement, imitating mouth or tongue movements, silly faces, or being unable to throw a ball at a target. Difficulty moving from sitting to moving under structures, crawling through a tunnel
- unable or very clumsy with jumping, climbing, moving between different level surfaces, climbing ladder to slide
- unable to take turns in play activities such as rolling ball back to you, stacking blocks
- seems fixated on the television, tablet, or phone and unable to engage with other toys in play
- difficulty putting things together such as connecting blocks, lacing, and beads
- unable to tolerate play on a swing, on a slide
- unable to play near or with other children
- unable to tolerate tactile messy play or engagement with media like play-doh, finger paint, or shaving cream
- difficulty removing pull on clothing from dress-up activities
Play is one of the most significant areas that can provide clues about your toddler’s development. As we’ve outlined, there is so much growth happening during this time. If you see your child struggling in any of the areas we mentioned, occupational therapy can help develop and strengthen the skills needed for learning.
Occupational therapists are experienced experts and can help identify the areas inhibiting your child’s primary occupation and introduce fun activities for successful skill development.
Children are tiny individual humans with varied interests and gifts. We embrace and work together with parents to help children reach their greatest potential.
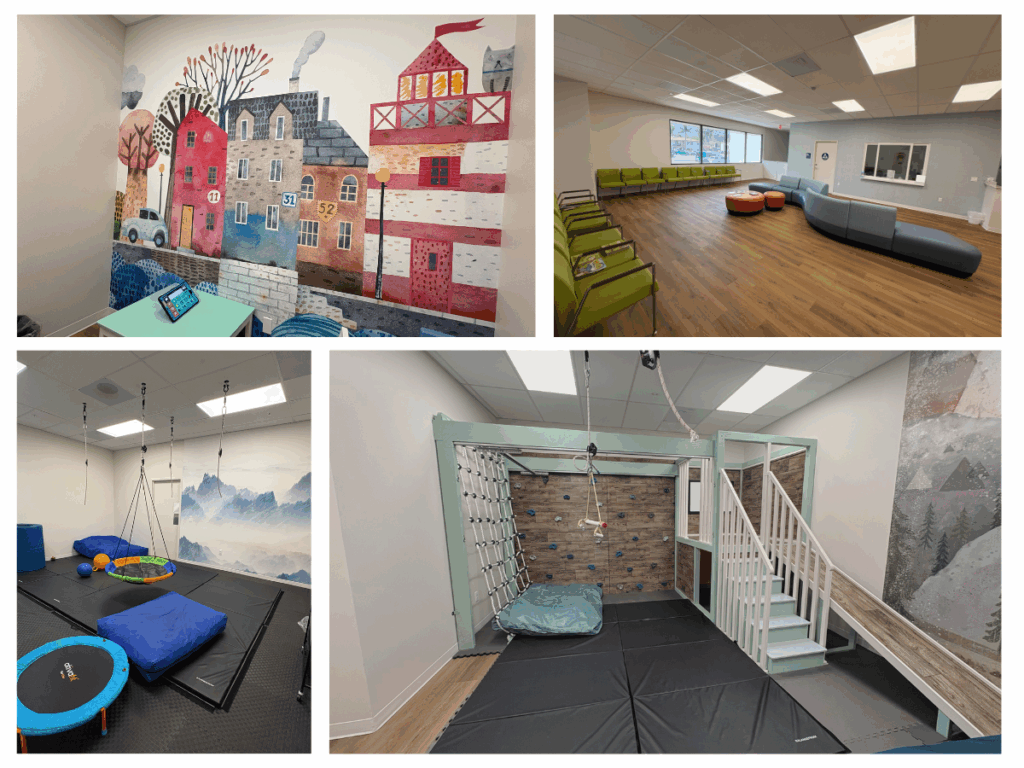
Come in and check us out in April for Occupational Therapy month!
Author: Pamela Vasiloff, OT